The Most Important Points at a Glance:
In this article, we've summarized for you:
- Which pathogens can be dangerous for you and your baby during pregnancy
- Which foods you should avoid and why
- Which micronutrients are important when planning for pregnancy and during pregnancy
- What to look for when purchasing supplements
Positive Pregnancy Test? Here’s What You Should Know While Waiting for Your Doctor’s Appointment!
Did you get a positive pregnancy test but still have to wait 1-2 weeks for your appointment at the gynecologist? We recommend that you start familiarizing yourself with the basics of proper nutrition right away. After all, you're not just nourishing yourself anymore, but also your baby.
Through the umbilical cord, your baby receives essential vitamins and nutrients—but can also absorb harmful substances. Your doctor will provide detailed guidance, but since appointment time is often limited, we’ve summarized the most important information for you here in a clear and concise way.
Even if you’re not feeling up to eating right now, this topic is more important than ever! 💛
Which Foodborne Infections Are Dangerous Right Now?
The Reason to Avoid Certain Foods During Pregnancy
The reason you should avoid certain foods during pregnancy is to prevent foodborne infections that could harm your unborn child. While these pathogens are usually harmless to you, they can often have serious consequences for your baby.
The following pathogens are particularly important to consider:
Which Pathogens Cause Dangerous Infections During Pregnancy?
These Pathogens Are Dangerous for You and Your Baby During Pregnancy.
What Is Toxoplasmosis?
Toxoplasmosis is a common infectious disease caused by the parasite Toxoplasma gondii. The primary host of this pathogen is the cat. The parasite is excreted in cat feces, contaminating soil and entering the food chain. The most common sources of transmission include:
- Raw or undercooked meat
- Unwashed fruits and vegetables
Transmission to the Unborn Child
If a mother is infected for the first time during pregnancy, the parasite can be transmitted to the fetus. An infection is particularly dangerous in the first or second trimester, as the baby's immune system is still developing and cannot effectively fight the parasite.
Possible Consequences for the Baby
Toxoplasmosis can cause miscarriage or stillbirth. Babies who survive the infection may suffer from severe health problems, such as:
- Vision impairment or blindness (e.g., retinal inflammation leading to severe visual impairment or blindness)
- Brain malformations & seizures (e.g., hydrocephalus, intellectual disabilities, epilepsy)
- Inflammation of organs such as the liver, spleen, and lungs
Symptoms to Watch For
If you are pregnant and experience any of the following flu-like symptoms, you should see your gynecologist for a simple blood test:
- Swollen lymph nodes, especially in the neck area
- Headaches
- Mild eye inflammation (if the retina is affected)
How Can You Protect Yourself from Toxoplasmosis?
Since toxoplasmosis can have serious consequences during pregnancy, it is essential to take preventative measures:
✔ Hygiene: Wash your hands thoroughly, especially after handling raw meat, soil, or cat litter.
✔ Food preparation: Cook meat thoroughly and wash fruits and vegetables carefully.
✔ Avoid contact with cat feces: Pregnant women should avoid cleaning litter boxes, as cats are the primary hosts of the parasite.
It’s important to note that women who had toxoplasmosis before pregnancy usually develop antibodies, making them immune to reinfection. A test at your gynecologist’s office can determine if you already have immunity.
What Are Listeria?
Listeria (Listeria monocytogenes) are bacteria that are widely found in the environment and can be transmitted through contaminated food. For healthy individuals, Listeria infections are usually harmless, causing only mild flu-like symptoms.
How Are Listeria Transmitted to the Unborn Baby?
If a pregnant woman consumes contaminated food, the bacteria enter the digestive system and can spread into the bloodstream. Once in the mother’s blood, Listeria can cross the placental barrier and infect the baby in the womb.
Possible Consequences for the Unborn Baby
A Listeria infection during pregnancy can lead to:
- Miscarriage or stillbirth (especially in the first and second trimester)
- Preterm birth (if infection occurs later in pregnancy)
- Neonatal Listeriosis, where the baby becomes infected in the womb or during birth, increasing the risk of:
- Sepsis (blood poisoning)
- Meningitis (inflammation of the brain lining)
Symptoms to Watch For
A Listeria infection (Listeriosis) is often mild or asymptomatic in healthy adults. However, pregnant women belong to the high-risk group due to changes in the immune system. Symptoms may resemble the flu or a gastrointestinal infection, including:
- Fever and chills
- Muscle aches
- Nausea, vomiting, or diarrhea
How to Protect Yourself from Listeria?
Listeria can be found in:
- Raw milk cheese (e.g., soft cheeses like Brie, Camembert, Feta)
- Raw meat or cold cuts (e.g., steak tartare, salami, Mett)
- Raw or smoked fish (e.g., sushi, smoked salmon)
To reduce the risk, follow these food safety measures:
✔ Cook meat, fish, and eggs thoroughly (core temperature of at least 70°C for 2 minutes)
✔ Wash or peel fruits and vegetables before consumption
✔ Consume only pasteurized dairy products
✔ Eat food as fresh as possible and reheat leftovers properly
✔ Practice good hygiene:
- Wash hands thoroughly and regularly
- Clean kitchen utensils frequently
- Store raw meat and fresh foods separately
- Regularly clean your refrigerator
By following these precautions, you can minimize the risk of Listeria infection during pregnancy.
What Are Salmonella and Coli Bacteria?
Salmonella and Coli bacteria (Escherichia coli, E. coli) are both bacteria that can infect the gastrointestinal tract and are often associated with foodborne infections. However, they differ in their effects and the diseases they can cause.
1) Salmonella (Salmonella enterica)
Transmission: Mostly through contaminated food, particularly animal products such as:
Raw or undercooked eggs
Raw poultry or meat
Unpasteurized dairy products
2) Coli Bacteria (Escherichia coli, E. coli)
Transmission: Usually through contaminated food, water, or smear infections, meaning contact with:
Contaminated surfaces, objects, or body parts
Raw or undercooked meat, raw fish, unpasteurized milk products.
How Do Salmonella and Coli Bacteria Affect the Unborn Baby?
Salmonella:
While the mother may suffer from vomiting, diarrhea, and fever, leading to fluid loss and nutrient deficiency, the baby may experience:
- Preterm birth: High fever and dehydration can trigger premature labor.
- Growth disorders: If the mother suffers from severe diarrhea and vomiting, she may not absorb enough nutrients.
- Baby infection: In rare cases, Salmonella can cross the placenta, leading to miscarriage or stillbirth, especially if the mother develops sepsis.
Coli Bacteria:
Different E. coli strains can produce toxins that may cause:
Bloody diarrhea and kidney damage in the mother (e.g., EHEC infection with HUS syndrome)
Bladder infections that may develop into kidney infections
For the baby, this can lead to:
- Preterm birth: If the mother is weakened by severe diarrhea or a kidney infection.
- Kidney damage: If the mother has an EHEC infection with HUS syndrome.
- Placenta infection: In rare cases, bacteria can infect the placenta, leading to miscarriage or stillbirth.
How Can You Protect Yourself from Salmonella and Coli Bacteria?
✔ Avoid raw meat, unpasteurized milk, and contaminated foods or ensure they are fully cooked.
✔ Wash fruits and vegetables thoroughly before eating.
✔ Wash your hands regularly, especially after using the restroom or handling raw food.
✔ See a doctor early if you experience urinary tract infections during pregnancy.
✔ Maintain good kitchen hygiene:
- Wash hands and cutting boards thoroughly after handling raw meat.
- Store raw and cooked foods separately to prevent cross-contamination.
By following these precautions, you can reduce the risk of Salmonella and E. coli infections during pregnancy.
Sources of infection & harmful foods
The following foods are often the carriers of the pathogens described above.
Consuming raw meat and unpasteurized dairy products can expose you and your unborn child to harmful bacteria, like listeria. Exposure to this type of bacteria can potentially result in premature birth or even stillbirth. Additionally, the Toxoplasma gondii parasite, transmitted through raw meat, cat feces, unwashed produce, or contaminated soil, can lead to toxoplasmosis and will pose a serious threat to your child if you contract it during pregnancy. It's crucial to fully cook all meat dishes to eliminate these risks. Avoid consuming anything raw or smoked. This means not just refraining from eating foods like mettwurst, raw ham, carpaccio, and mett, but also avoiding salami and liverwurst during pregnancy. Opt for cooked sausages like Fleischwurst, mortadella, and boiled ham, as cooking kills these harmful germs.
Always make sure that any fish you consume is fully cooked through. Avoid sushi, sashimi, and oysters. Cold-smoked or pickled fish products such as trout, salmon or herring are also on the list of foods to avoid during pregnancy because they can be riddled with listeria.
It's important to avoid consuming cheeses labeled as "raw milk" or "premium milk," including soft cheeses and semi-hard cheeses like Camembert, due to the potential risk of Listeria infection. However, you can safely enjoy soft cheeses made from pasteurized milk and hard cheeses. It's recommended to steer clear of red mold cheeses such as Esrom, Handkäse, or Tilsiter, as well as shredded cheese from the refrigerated section.
When preparing eggs and egg-based dishes, make sure that they are well cooked, because raw eggs can contain salmonella. Caution: raw eggs are often found in homemade dishes such as tiramisu, mousse au chocolat, mayonnaise, hollandaise sauce, and ice cream. Industrially manufactured products, on the other hand, are harmless because they only contain pasteurised eggs that have been sufficiently heated.
Even small amounts of alcohol can harm your unborn baby and lead to birth defects. That's why alcohol is absolutely taboo during pregnancy! If you consume alcohol during pregnancy, you can trigger FASD (Fetal Alcohol Spectrum Disorder) in your child. If your child is affected, it can cause lifelong damage to their motor skills and/or mental impairment.
Foods that contain alcohol
You should also note that some foods and dishes may also contain alcohol.
Cooking with alcohol
When cooking at home, you should simply leave the alcohol out, as residual alcohol will remain even after the liquid has been boiled away.
Alcohol-free drinks
Watch out; even beverages that are labeled as non-alcoholic may actually contain alcohol. According to regulations, a beverage can be labeled as non-alcoholic even if it contains up to 0.3 percent residual alcohol. That's why it's also important to drink these kinds of beverages responsibly.
Not only are they sweet and contain unhealthy additives, but they also have too much caffeine for pregnant women. For example, if you like to drink cola, you should limit your consumption to a maximum of two glasses a day. Drinks containing quinine, such as tonic water or bitter lemon, should only be consumed in moderation, if at all. Quinine is a natural plant toxin that, in large amounts, can cause vomiting, blurred vision, and even premature labor.
Honey is one example of a food that raises uncertainties regarding nutrition during pregnancy. Experts caution against giving honey to babies under the age of one because it can potentially contain the bacterium Clostridium Botulinum (according to Wikipedia). The stomach acid present in a pregnant woman's body rapidly neutralizes the bacterium, posing no threat to the baby in the womb. Honey, abundant in various trace elements and vitamins, becomes a valuable nutritional source during pregnancy. Nonetheless, due to its elevated sugar content, expectant mothers should limit their intake to a small quantity – no more than one teaspoon per day.
The Most Important Vitamins and Micronutrients You Need During Pregnancy
If you already eat a varied and balanced diet, your baby will receive almost everything it needs.
However, the demand for certain micronutrients—such as folic acid, iodine, omega-3, vitamin D, choline, and, in many cases, iron—is so high during pregnancy that it cannot be met through diet alone. In these cases, supplementation is recommended.
Your doctor will advise you on what is specifically relevant for you.
Here’s an overview of the most important nutrients and their benefits at a glance:
Why Do You Need More Folic Acid During Pregnancy?
Folic acid plays a crucial role in cell growth and is essential for the development of your baby’s brain, neural tube, and spinal cord. Adequate intake is important not only during pregnancy but also before conception to support healthy development from the very beginning.
Which Foods Contain Folic Acid?
Folic acid (or folate) is primarily found in:
✔ Green vegetables (e.g., spinach, lettuce, kale, fennel, cucumbers, tomatoes)
✔ Legumes (e.g., lentils, chickpeas, soybeans)
✔ Whole grains & wheat germ
✔ Potatoes & nuts
✔ Oranges
How Much Folic Acid Do You Need During Pregnancy?
- Before Pregnancy (if already supplementing): 800 mcg daily (starting at least 3–4 months before conception)
- During Early Pregnancy (up to week 12): 800 mcg daily
- From Week 13 Onward: 400 mcg daily
If you haven't been taking folic acid before pregnancy, it's recommended to start with 800 mcg as soon as you know you're pregnant and reduce to 400 mcg after the 12th week.
Why Supplementation?
Getting enough folic acid through diet alone is difficult. To avoid additional stress, taking a high-quality natural supplement ensures you meet your daily needs. Your doctor will advise you on the exact dosage.
What Should You Consider When Taking Folic Acid?
Opt for bioactive folic acid (L-methylfolate).
This form is immediately absorbed by the body and does not need conversion, making it more effective than synthetic folic acid.
When Should You Take Folic Acid?
- Best taken in the morning on an empty stomach with water or orange juice (Vitamin C enhances folic acid absorption).
- If you have a sensitive stomach, take it with a meal.
- If you're also taking iron supplements, wait at least two hours between doses, as iron can inhibit folic acid absorption.
When to Start Taking Folic Acid?
Ideally, 3–4 months before trying to conceive to build up folic acid levels in the body.
For more detailed scientific information, refer to:
📖 Scholl, T.; Johnson, W. G. (2000) - Folic Acid: Influence on the Outcome of Pregnancy (American Journal of Clinical Nutrition, 71(5), 1295S-1303S)
📖 Cui, Y.; Liao, M.; Xu, A.; et al. (2021) - Association of Maternal Pre-Pregnancy Dietary Intake with Adverse Maternal and Neonatal Outcomes (Czech Journal of Food, 63(1))
📖 Nishigori, H.; Nishigori, T.; Obara, T.; et al. (2023) - Prenatal Folic Acid Supplementation and Cognitive Development in Children (Scientific Reports, 13(1), 9541)
Why Do You Need More Iodine During Pregnancy?
Iodine is an essential trace element that plays a crucial role during pregnancy, especially in the first trimester. It is vital for the development of your baby’s thyroid, brain, and overall growth.
Your baby cannot produce its own thyroid hormones in the first weeks of pregnancy, making it entirely dependent on your iodine supply.
Which Foods Contain Iodine?
Iodine is naturally found in:
✔ Fatty sea fish (e.g., cod, haddock, tuna)
✔ Seaweed & seafood
✔ Iodized salt
✔ Dairy products (e.g., milk, yogurt, cheese)
✔ Bread & cold cuts
How Much Iodine Do You Need During Pregnancy?
Daily iodine requirement:
Adults: 230 mcg/day
Pregnant & breastfeeding women: 260 mcg/day (according to the German Nutrition Society (DGE))
Since many iodine-rich foods are limited during pregnancy, a supplement is often recommended to ensure you and your baby get enough iodine.
What Should You Consider When Choosing an Iodine Supplement?
✔ Bioavailability matters – iodine from supplements should be easily absorbed by the body.
✔ Seaweed-based products can contain excessively high iodine levels, so always check the dosage.
When Is the Best Time to Take Iodine?
- Morning is ideal – your thyroid is most active in the morning and produces more hormones at this time.
- Take iodine with fat or protein (e.g., dairy products, eggs) to improve absorption.
- Avoid taking iodine on an empty stomach – some people experience stomach discomfort if they take it without food.
- Iron deficiency can inhibit iodine absorption – if you have an iron deficiency, your doctor will guide you on how to balance both nutrients.
Why Do You Need Omega-3?
Omega-3 fatty acids are essential unsaturated fatty acids that your body cannot produce on its own.
The two most important forms of Omega-3 for pregnancy are:
✔ DHA (Docosahexaenoic acid): Essential for brain development, vision, memory, and nerve cells.
✔ EPA (Eicosapentaenoic acid): Has anti-inflammatory properties and supports the cardiovascular system and immune system.
Which Foods Contain Omega-3?
Omega-3 fatty acids are naturally found in:
✔ Fatty fish (e.g., salmon, herring, mackerel, sardines)
✔ Plant-based sources (e.g., algae, flaxseed oil, chia seeds, walnuts)
How Much Omega-3 Do You Need?
According to the German Nutrition Society (DGE), pregnant and breastfeeding women should consume:
✔ At least 200 mg DHA & EPA daily
✔ Ideally 400–800 mg DHA & EPA per day
To meet this requirement, the DGE recommends eating fatty sea fish (e.g., herring, mackerel, sardines) 1–2 times per week.
Alternative option: If consuming fish is difficult (especially in early pregnancy), high-quality Omega-3 supplements can help.
For those concerned about the fishy aftertaste, plant-based sources like algae oil are a great alternative.
What Should You Look for When Buying Omega-3 Supplements?
✔ Look for DHA & EPA (bioavailable forms of Omega-3).
✔ Algae oil is the best alternative – free from mercury and toxins, making it a safe choice for pregnancy.
✔ Ideal ratio for pregnant and breastfeeding women: 1:2 EPA/DHA.
When Should You Take Omega-3?
- Omega-3 can be taken throughout the day.
- For better absorption, take it with a fat-containing meal (e.g., avocado, nuts, healthy oils), as DHA & EPA are fat-soluble.
- Taking Omega-3 in the evening may support better sleep.
Why Is Iron Important?
Iron is primarily needed for the production of red blood cells, which supply oxygen to you and your baby. During pregnancy, your body produces more blood to support your baby’s development, which significantly increases your iron needs.
Which Foods Contain Iron?
Iron is found in:
✔ Liver (note: liver should be avoided in early pregnancy due to high vitamin A content)
✔ Wheat bran & quinoa
✔ Pumpkin seeds & sesame seeds
✔ Legumes (e.g., lentils, chickpeas)
✔ Flaxseeds & pistachios
How Much Iron Do You Need Daily?
According to the German Nutrition Society (DGE):
✔ Pregnant & breastfeeding women: 20–30 mg iron per day
✔ Non-pregnant adults: 10–15 mg per day
If you have acute iron deficiency, you may need an iron supplement to replenish your stores.
Signs of Iron Deficiency in Pregnancy
Since fatigue, exhaustion, and lack of energy are common in early pregnancy, iron deficiency can be difficult to detect. However, symptoms to watch for include:
- Extreme fatigue & low energy
- Difficulty concentrating
- Sleep disturbances
- Headaches
Don't stress—your gynecologist regularly checks your iron levels and will inform you if supplementation is necessary.
What Should You Consider When Choosing an Iron Supplement?
Not all iron supplements are the same—different forms have varying absorption rates (bioavailability):
✔ Well-tolerated & highly absorbable forms:
- Iron(II)-bisglycinate → Highly bioavailable, well tolerated
- Iron fumarate → Good absorption, moderate tolerance
- Iron gluconate → Good bioavailability, better tolerated than sulfate
When Should You Take Iron?
- Best taken in the morning on an empty stomach, as iron is absorbed best this way.
- Take iron with vitamin C (e.g., a glass of orange juice) to enhance absorption.
Avoid taking iron with:
- Coffee, tea, or dairy products, as they inhibit iron absorption.
- Calcium, magnesium, and zinc supplements, as they interfere with iron uptake—wait a few hours between doses.
Why Do You Need Choline?
Choline is an essential nutrient that plays a crucial role during pregnancy in:
✔ Brain development of the baby
✔ Liver health and detoxification
✔ Cell formation and placental function
It belongs to the B-vitamin family and is often overlooked, despite being just as important as folic acid for mother and baby.
📌 Choline is vital for the production of the neurotransmitter acetylcholine, which supports memory and cognitive development.
📌 Like folic acid, choline is essential for the closure of the neural tube (spinal cord & brain).
📌 It also helps form cell membranes, supports healthy fetal growth, and promotes placental blood circulation, ensuring optimal nutrient supply to the baby.
Which Foods Contain Choline?
✔ Eggs (especially the yolk)
✔ Liver (beef liver, in moderation during pregnancy)
✔ Meat & poultry
✔ Fish (e.g., salmon, cod)
✔ Legumes (e.g., chickpeas, lentils)
✔ Nuts & seeds (e.g., sunflower seeds, peanuts)
How Much Choline Do You Need During Pregnancy?
📌 Pregnant women: 450 mg per day
📌 Breastfeeding women: 550 mg per day (since the baby gets choline through breast milk)
Many pregnant women—especially vegetarians and vegans—struggle to get enough choline through diet alone. In these cases, supplementation is recommended, in consultation with a doctor.
What to Consider When Choosing a Choline Supplement?
✔ High bioavailability is important for better absorption and utilization.
Good choline forms include:
- Choline bitartrate
- Alpha-GPC (Alpha-Glycerophosphocholine)
When & How Should You Take Choline?
- Choline is best absorbed when taken with a meal, especially one that contains healthy fats (e.g., eggs, avocado, nuts).
- Choline can be taken at any time of the day, but consistency is key.
- If you are supplementing, look for phosphatidylcholine or choline bitartrate—these forms are well absorbed by the body.
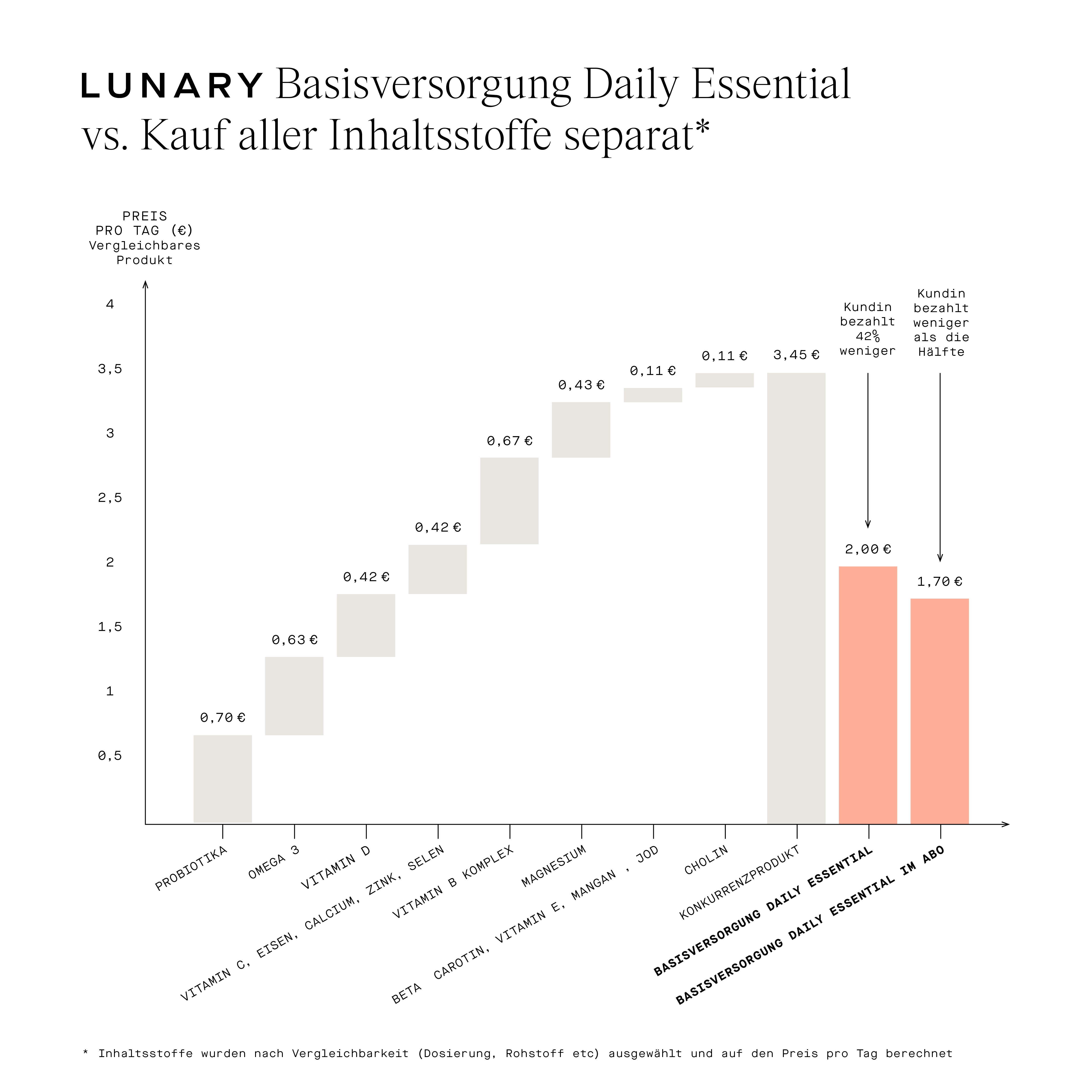
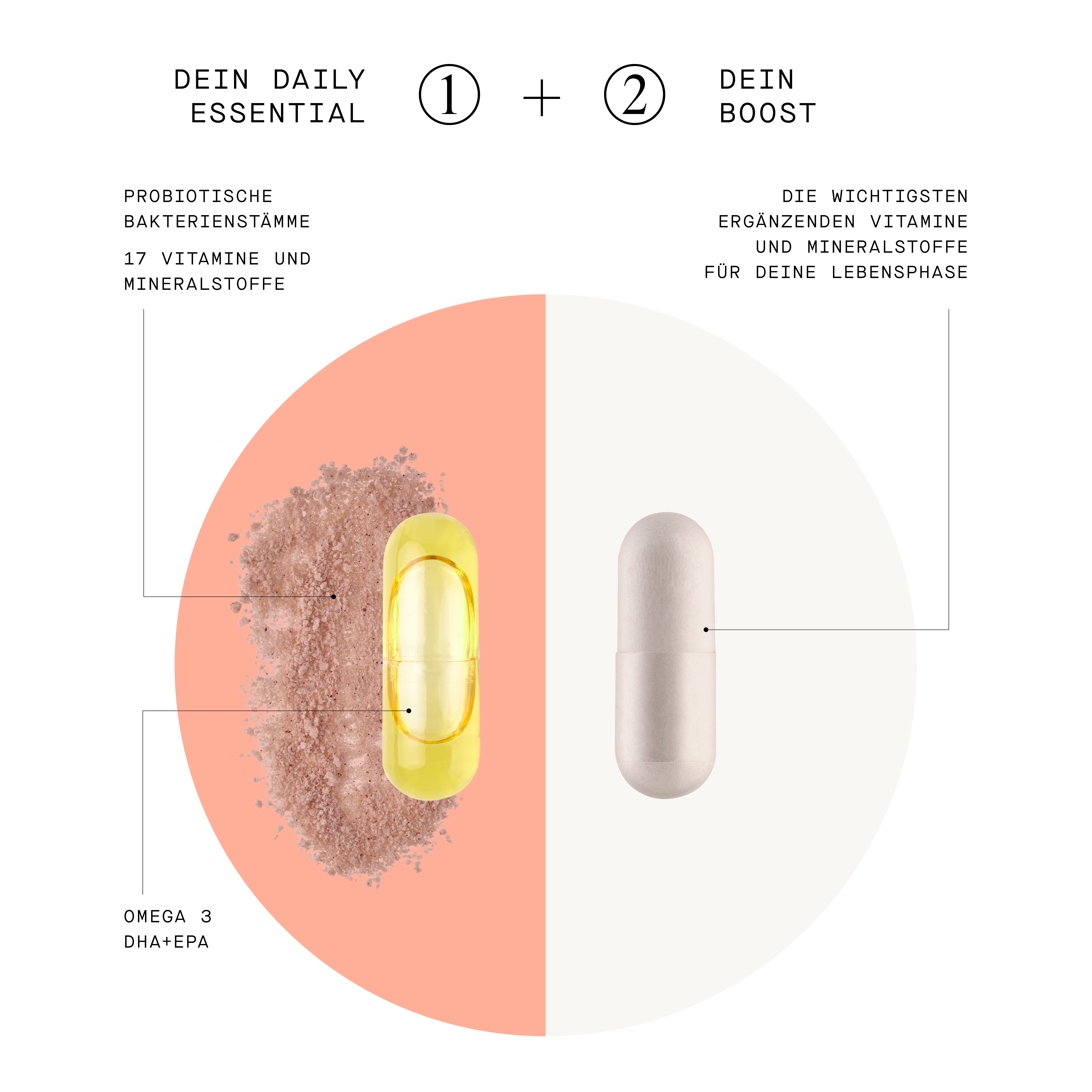
LUNARY - Complete Nutrient Support for You and Your Baby
Because proper nutrient intake is essential for both you and your baby, we have included a brand that provides comprehensive support with all the essential nutrients.
LUNARY is a brand that places great importance on ingredient origin, quality, and bioavailability, ensuring that your body receives only the best.
✔ Specifically designed for the needs of the female body, LUNARY is perfectly tailored to support you throughout your pregnancy and beyond.
But don't worry: if just the sight or smell of food that you may have loved in the past has you running to the bathroom - don't stress! Your baby will not be undernourished right away if your diet now seems a bit one-sided. When it's hard to keep anything down, and morning sickness is overtaking everything, a balanced diet seems like a distant fantasy. It's important to realise that you are not alone! We have gathered all the important tips and tricks for you below.
Podcast
Hebammensalon (Midwife Salon)

Healthy
Smoothies by us for you
Have you already discovered our smoothie recipes? Since the postpartum time is sacred to us, we have developed smoothies that are specifically tailored to the needs of your body during this time. Since they are based on super foods, they can't hurt you during pregnancy.
Try them out and report back. We are really excited and hope you are too!